Crusty, itchy, red eyes? There is a decent chance you could have conjunctivitis, or pink eye, an infection of the thin lining around the eye and the eyelid, caused by bacteria, an allergen, virus, or even your contact lenses. Whatever the cause — you call up your doctor to get a prescription to clear it up, right? Not really.
About six million people are impacted by pink eye in the US each year. If you have children, you probably know to keep your child home from school if they have symptoms. Viral and bacterial pink eye are both highly contagious and can spread quickly through shared items, coughing, sneezing, or personal contact. Often parents are required to keep a child home until they have no symptoms, or until they have a prescription for antibiotic eye drops. This well-intentioned but poorly informed policy encourages parents to insist on a prescription to get their child back in school.
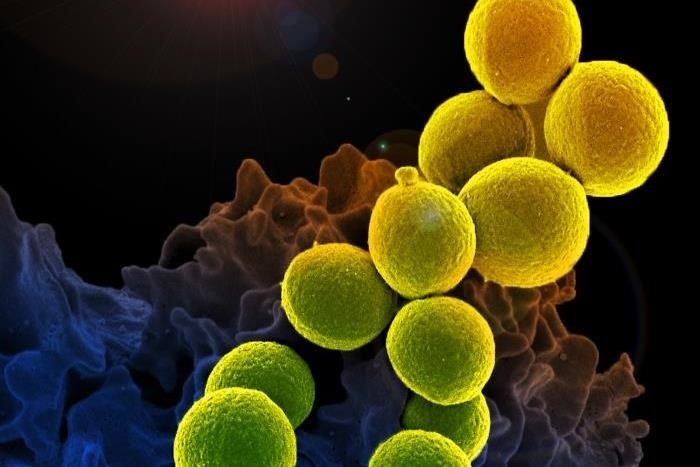
A recent study published in the journal Opthalmologist finds many healthcare providers are overprescribing antibiotics for pink eye, adding to the problem of antibiotic resistant pathogens and maybe even delaying recovery from the infection.
What Is the Problem with Treating Pink Eye with Antibiotics?
Pink eye is the most common eye infection encountered in everyday medical settings. While half of pink eye cases are seen in family doctor offices, about one-third of emergency department visits concerning the eyes resulting in a diagnosis of pink eye. While pink eye, or acute conjunctivitis, is uncomfortable, it does not usually require antibiotics to clear up on its own. Antibiotics are wasted on viral causes of pink eye, which account for almost 60% of pink eye diagnosis. Both viral and bacterial pink eye are relatively mild, and both clear the body within seven to 14 days without medical intervention.
On the flip side, treating routine pink eye infections of either viral or bacterial with antibiotics can irritate the eye, worsening of viral infections in some cases, and hastening the development of antibiotic-resistant pathogens.
In a large study involving 340,372 members of a national US managed care network, scientists from the University of Michigan Kellogg Eye Center crunched the numbers on patients who filled prescriptions after being evaluated for acute conjunctivitis, pink eye, between the years 2001 and 2014. After looking at those numbers — the researchers then considered factors that may have influenced some patients to fill those prescriptions, while others did not.
The results give rise to questions about why healthcare practitioners are offering so many prescriptions to patients who probably do not need the cost, or risk, of antibiotics. Some of the findings include:
- The gender of participants was almost equal (58% of the participants were women), the racial composition included white, black, Asian, and Latino.
- Among those diagnosed with pink eye, 58% filled one or more prescriptions for the infection within the 14-day period that followed the diagnosis.
- Patients that filled prescriptions tended to be younger, around 35 years, as opposed to those who were older, around 45-plus years. Those who filled the prescriptions tended to have higher incomes and more education. Patients on Medicare Advantage plans, mostly older than 66 years of age, were significantly less like to fill the prescriptions.
- About 20% of those who filled prescriptions received medications that were a combination of antibiotic and corticosteroid. The combinations are known to prolong viral infections, increase viral shedding, and possibly reactivate latent eye infections caused by herpes simplex infections.
- People who might have been more likely to suffer a serious infection, such as those with diabetes or HIV/AIDS, and contact lens wearers, were not more likely to fill prescriptions they received for pink eye.
Part of the problem of over-prescribing antibiotics involves similarity of symptoms. Some physicians may be unable to diagnose the cause of acute conjunctivitis, and opt for an antibiotic "just to be safe." In this study, patients that were white, affluent, and had more education were more likely to fill the unneeded prescriptions — which could reflect a demand or request by the patient for the prescription to minimize the inconvenience of the infection and speed recovery — neither of which antibiotics are likely to help.
In a press release, lead author Nakul Shekhawat, with the University of Michigan Health System notes:
This study opens the lid on overprescribing of antibiotics for a common eye infection. It shows that current treatment decisions for pink eye are not based on evidence, but are often driven more by the type of health care practitioner making the diagnosis and the patient's socioeconomic status than by medical reasons. The potential negative consequences are difficult to justify as we move toward focusing on value in health care.
Overall, the study authors suggest increased efforts to educate administrators who create school policies, and encourage healthcare providers to reduce unnecessary prescription of unneeded, and potentially harmful, antibiotics.
Just updated your iPhone? You'll find new emoji, enhanced security, podcast transcripts, Apple Cash virtual numbers, and other useful features. There are even new additions hidden within Safari. Find out what's new and changed on your iPhone with the iOS 17.4 update.
























Be the First to Comment
Share Your Thoughts